SHRADHA PAL
KATHMANDU: Get married soon, time is running out, if you marry late (30’s is the dreaded age), you won’t be able to conceive’ — such naggings never stop till the daughter succumbs to parents’ wishes. But is it true? Is it risky to conceive when you are in your 30’s? Society says yes, but the doctor disagrees.
“It is not true. The egg count will lessen as you age, but there is a possibility to become pregnant,” clears Dr Bimala Lakhey, Sr Consultant Obstetrician Gynaecologist.
Despite this information people may still be sceptical as old habits die hard. Therefore, relating to the pressures a woman faces, is it a good idea to become pregnant during mid 30’s? Nepali society is such that many women are financially dependent on their husbands, so if a woman marries late followed by pregnancy, it is a sound decision. “If a woman opts to be pregnant in her 30’s, then she is emotionally ready to handle the responsibility and is financially secure, so I support this decision,” encourages Dr Lakhey.
Some risks
With this you also have to understand that till the age of 35 there won’t be any problems as such, but after that there can be complications, which should be noted.
Some risk or complications are —
• Low birth rate.
• Chances of miscarriage — “If in 20’s chances of miscarriage is 25 per cent, in 40’s it is double due to chromosomal abnormality,” says Dr Lakhey.
• Child can suffer from Down’s syndrome.
• As the egg count is less in this age group, becoming pregnant may take longer.
• Chances of having twins increase. “This is because of egg increasing medicine.”
• Developing high blood pressure, which is an age factor.
“Nonetheless, it is not alarming though comparatively to younger age, the complications can be more,” adds Dr Lakhey. There are treatments and diagnosis that can deal with such issues.
Also good health will help before you conceive, for which you need to eat food with folic acid content “present in green vegetables”, a balanced diet also becomes important, limiting your caffeine consumption, exercising regularly, not drinking alcohol and not smoking.
Talking about pregnancy, the role of the biological father is also important to mention. “If the father is more than 50 years old, then the child born will have chances of being autistic,” says Dr Lakhey.
So what after the pregnancy?
“She has to be alert about the diabetes and has to be under constant medical supervision, also screening test should be conducted to check chromosomes,” answers Dr Lakhey.
Other than that one need not worry.
Boon of medical
science
When one door closes, the other opens. If it doesn’t work naturally for you, then there is an alternative — In Vitro Fertilisation (IVF).
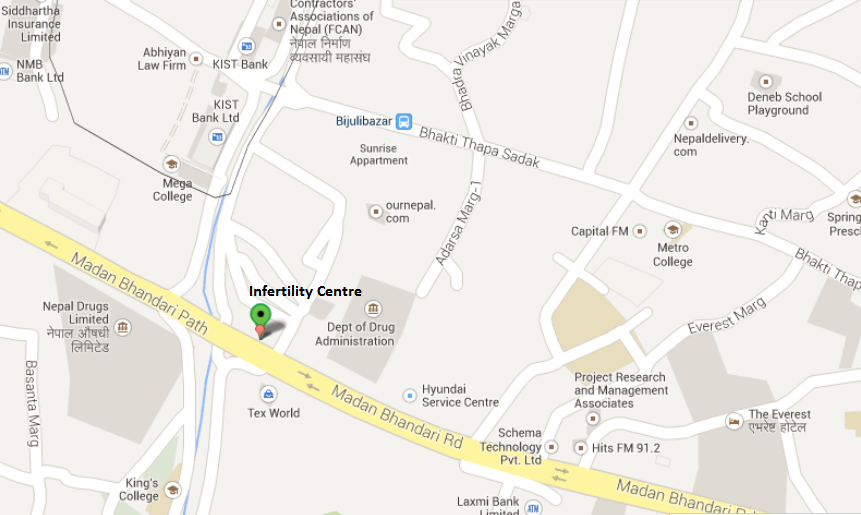
So who should opt for this process? “There are many indications for IVF,” says Dr Uma Shrivastava, Infertility and IVF Specialist and Director at Infertility Centre, Bijulibazar, New Baneshwor which are —
1. If both the fallopian tubes are blocked.
2. Male infertility
3. Failed IVF
4. Failed conventional treatment
5. Failed ovulation
6. Endometriosis
7. Unexplained infertility
This is definitely a boon of medical science, but Dr Shrivastava asserts that it shouldn’t be fashion, which is the trend these days. This process is a blessing for many, but to understand every aspect is also equally important. There are complications of IVF, “which should be highlighted,” asserts the doctor, such as —
• Multiple pregnancy
• Ovarian Hyperstimulation Syndrome (OHSS) in Polycystic Ovarian Syndrome (PCOS), “which can also lead to death,” warns Dr Shrivastava.
• Other hormonal complications like increasing cyst and failed stimulation, “where after one IVF, the woman can go into early menopause”, which means she can never become pregnant.
The more knowledge you have, the better decisions you can make. Therefore, before opting for IVF, proper hormone test is vital. You have to first visit the hormone specialist known as endocrinologist. After s/he gives the green signal, then it is the gynaecologist’s job and so the process moves forward.
However, not everyone can opt for IVF. If you have inactive ovary, do not think about IVF instead “you should take a donor egg,” suggests Dr Shrivastava. Another case is — if you have tumour in your uterus, an alternative for such women can be “surrogacy”.
Every woman at some point of her life wants to be a mother, when she is ready. Or what is wrong if she doesn’t want to be pregnant? More than science or societal pressure, ultimately the choice should to be hers!
Article Published on The Himalayan Times
2012-09-17
“It is not true. The egg count will lessen as you age, but there is a possibility to become pregnant,” clears Dr Bimala Lakhey, Sr Consultant Obstetrician Gynaecologist.
Despite this information people may still be sceptical as old habits die hard. Therefore, relating to the pressures a woman faces, is it a good idea to become pregnant during mid 30’s? Nepali society is such that many women are financially dependent on their husbands, so if a woman marries late followed by pregnancy, it is a sound decision. “If a woman opts to be pregnant in her 30’s, then she is emotionally ready to handle the responsibility and is financially secure, so I support this decision,” encourages Dr Lakhey.
Some risks
With this you also have to understand that till the age of 35 there won’t be any problems as such, but after that there can be complications, which should be noted.
Some risk or complications are —
• Low birth rate.
• Chances of miscarriage — “If in 20’s chances of miscarriage is 25 per cent, in 40’s it is double due to chromosomal abnormality,” says Dr Lakhey.
• Child can suffer from Down’s syndrome.
• As the egg count is less in this age group, becoming pregnant may take longer.
• Chances of having twins increase. “This is because of egg increasing medicine.”
• Developing high blood pressure, which is an age factor.
“Nonetheless, it is not alarming though comparatively to younger age, the complications can be more,” adds Dr Lakhey. There are treatments and diagnosis that can deal with such issues.
Also good health will help before you conceive, for which you need to eat food with folic acid content “present in green vegetables”, a balanced diet also becomes important, limiting your caffeine consumption, exercising regularly, not drinking alcohol and not smoking.
Talking about pregnancy, the role of the biological father is also important to mention. “If the father is more than 50 years old, then the child born will have chances of being autistic,” says Dr Lakhey.
So what after the pregnancy?
“She has to be alert about the diabetes and has to be under constant medical supervision, also screening test should be conducted to check chromosomes,” answers Dr Lakhey.
Other than that one need not worry.
Boon of medical
science
When one door closes, the other opens. If it doesn’t work naturally for you, then there is an alternative — In Vitro Fertilisation (IVF).
So who should opt for this process? “There are many indications for IVF,” says Dr Uma Shrivastava, Infertility and IVF Specialist and Director at Infertility Centre, Bijulibazar, New Baneshwor which are —
1. If both the fallopian tubes are blocked.
2. Male infertility
3. Failed IVF
4. Failed conventional treatment
5. Failed ovulation
6. Endometriosis
7. Unexplained infertility
This is definitely a boon of medical science, but Dr Shrivastava asserts that it shouldn’t be fashion, which is the trend these days. This process is a blessing for many, but to understand every aspect is also equally important. There are complications of IVF, “which should be highlighted,” asserts the doctor, such as —
• Multiple pregnancy
• Ovarian Hyperstimulation Syndrome (OHSS) in Polycystic Ovarian Syndrome (PCOS), “which can also lead to death,” warns Dr Shrivastava.
• Other hormonal complications like increasing cyst and failed stimulation, “where after one IVF, the woman can go into early menopause”, which means she can never become pregnant.
The more knowledge you have, the better decisions you can make. Therefore, before opting for IVF, proper hormone test is vital. You have to first visit the hormone specialist known as endocrinologist. After s/he gives the green signal, then it is the gynaecologist’s job and so the process moves forward.
However, not everyone can opt for IVF. If you have inactive ovary, do not think about IVF instead “you should take a donor egg,” suggests Dr Shrivastava. Another case is — if you have tumour in your uterus, an alternative for such women can be “surrogacy”.
Every woman at some point of her life wants to be a mother, when she is ready. Or what is wrong if she doesn’t want to be pregnant? More than science or societal pressure, ultimately the choice should to be hers!
Article Published on The Himalayan Times
2012-09-17